GENERAL MEDICINE CASE
December 21 , 2021
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence base inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
A 70 year old patient came to OPD with chief complaints of
Burning micturition since 10 days
Shortness of breath since 10 days
Fever and chills since 10 days
History of present illness :
Patient was apparently asymptomatic 2 weeks back then he developed weakness for which he visited a hospital in nalgonda where the tests were done andbdiagnosed with kidney disease. Then he started using medication and due to which he developed fever and chills then he visited KIMS.
The normal routine of the patient 2 weeks ago was he used to wakeup 5'0 clock in the morning and do all the household work and then used to go for farming around 10 and then used to return home in the evening. 2 weeks back after the work he experienced weakness , pedal edema , burning micturition and stopped the work.
Past History :
The patient is not a known case of Diabetes
mellitus , Hypertension and asthma.
Known case of Tuberculosis 20 years back used
HAZE regimen for 6 months.
Family history :
No relevant family history
Medical history :
Not allergic to any known drugs
Personal history :
Diet - Mixed
Appetite - Reduced
Sleeping - Adequate
Bowel and bladder movement - Regular
Habits - chronic alcoholic since 20 years daily
180mL
Chronic smoker since 20 years 2-4 beedis per day
General examination :
Patient is conscious , coherent and cooperative
Well Oriented to time , place and person
Pallor is present
No icterus
No cyanosis
No clubbing
No edema
Pulse rate -69 / min
Blood pressure - 130 / 80 mmHg
Respiratory Rate - 16 cpm
SpO2 - 98% at room air
GRBS - 105 mg / dl
Systemic examination :
CVS :
S1 S2 heard
No thrills
No murmurs heard
RESPIRATORY SYSTEM :
No dyspnea
Wheezing is present
Trachea is in central position
Vesicular breath sounds heard
ABDOMEN :
Scaphoid in shape
No tenderness
No palpable mass
Normal hernial orifice
No free fluid
No bruits
Liver is not palpable
CNS :
Patient is conscious
Speech is present
Reflexes are normal
PROVISIONAL DIAGNOSIS
AkI ?
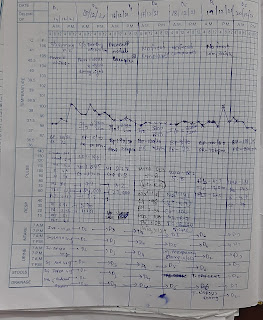
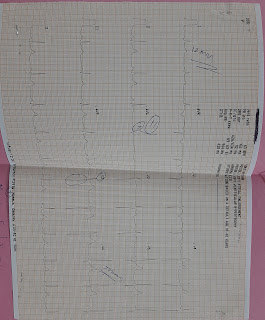
INVESTIGATION
Treatment :
1.INJ.LASIX 20 MG IV/BD
2.INJ PIPTAZ 4.5 GM IV/STAT
3.INJ.PANTOP 40 MG IV/SDS
4.INJ ZOFER 4 MG IV/STAT
5.NEB.BUDECORT 12 HRLY
DUOLIN 6 HRLY
6.STICT I/O CHARTING
7.BP,TEMPERATURE MONITORING 4 HRLY
2.INJ PIPTAZ 4.5 GM IV/STAT
3.INJ.PANTOP 40 MG IV/SDS
4.INJ ZOFER 4 MG IV/STAT
5.NEB.BUDECORT 12 HRLY
DUOLIN 6 HRLY
6.STICT I/O CHARTING
7.BP,TEMPERATURE MONITORING 4 HRLY

















Comments
Post a Comment