60 YEARS OLD FEMALE PATIENT WITH HISTORY OF BURNING MICTURAITION
CASE:
DATE OF ADMISSION:02/08/2021
60years old female resident of Hyderabad presented to the opd with chief complaint of burning micturaition since 2weeks
HISTORY OF PRESENT ILLNESS:
patient was apparently asympotmatic 14days back then she developed low backache,followed by fever ,chills, with raised bp levels and developed generalised weakness with burning micturaition.
PAST HISTORY:
she is having similar complaint every 6months since 6 years
History of hysterectomy surgery
No history of epilepsy,pedal edema
Having DM since 25yrs
PERSONAL HISTORY:
Appetite-less
Diet-mixed
No addictions
Bowel and bladder movements-normal
FAMILY HISTORY:
No history of similar complaints in family
TREATMENT HISTORY:
No history of drug allergy.
GENERAL EXAMINATIONS:
Patient is coherent ,conscience and cooperative
pallor-positive
No icterus
No cyanosis
No clubbing,lymphadenopathy
Temp-
BP-110/80 mm of Hg
PR-95 BPM
RR-23 CPM
GRBS-135 mg/dl
SYSTEMIC EXAMINATION;
CVS:S1,S2 heard
Respiratory system:
Inspiratory crepts noted
CNS:no alternation in cns
Per abdomen:
Soft,no tender
PROVISIONAL DIAGNOSIS:
Case of UTI with sepsis
INVESTIGATION:
Vitals and temp:
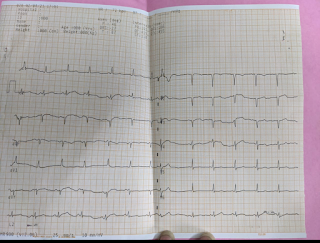
ECG:
USG KUB REGION:
ABG:
Hemogram:
CUE:
Serum urea,creatinine,electrolytes:
2/8/2021:
3/8/2021:
4//8/2021:
Serum creatinine:4.18
5/8/2021:
Urea:121
Serum creatinine:4.2
6/8/2021:
Urea:132
Serum creatinine:4.1
Reticulocyte count:
Treatment:
TAB PAN 40mg po/Of
Inj.levofloxacin 500mglv/od
Tab.tamsulosin 0.4mg po/hr
Tab.thyronom 50 microgram/po/of
Tab.ultracet1/2tab/po/of
Inj.piptaz 2.2g/iv/tid













Comments
Post a Comment